CITY OF SAN FERNANDO, Pampanga – The Philippine Health Insurance Corporation (PhilHealth) has intensified its efforts in processing claims and collecting employer contributions to ensure a stable healthcare system in Central Luzon.
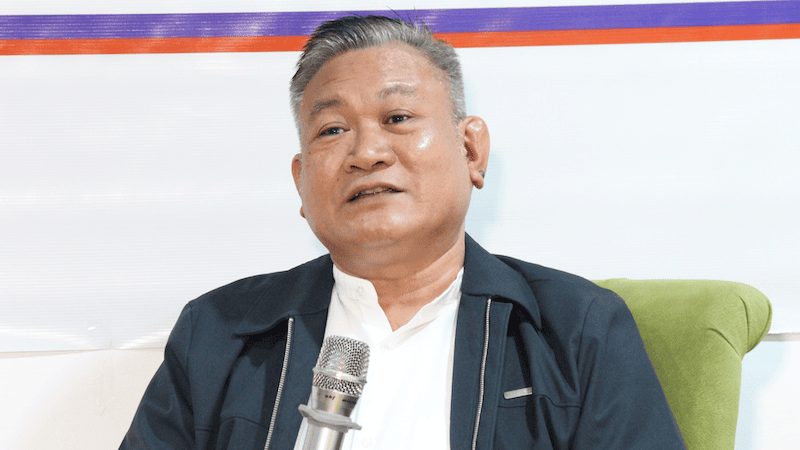
During the first episode of the Kapihan sa Bagong Pilipinas of the Philippine Information Agency for 2025, PhilHealth Regional Office III Acting Vice President Henry Almanon said the agency had a P6.23 billion collection from private employers and nearly P3 million recovered from delinquent employers in 2024 which can sustain the goals of Universal Health Care (UHC) and enhance hospital funding.
PhilHealth significantly sped up its claims processing, reducing turnaround to an average of 19 days from 26 days, ensuring uninterrupted quality healthcare services to the public.
“In Central Luzon, from January to December 2024, the agency paid P22 billion for benefit claims for the health services provided to members and dependents by our partner healthcare providers,” Almanon.
In addition, PhilHealth has raised its financial support for over 9,000 case rates, following a 30 percent increase last year and an additional 50 percent increase in 2025.
This reduces out-of-pocket expenses for members and allows hospitals to provide better services.
To ensure a sustainable fund for healthcare services, PhilHealth collected P6.23 billion from 11,679 private employers in 2024.
Additionally, the agency recovered nearly P3 million in premium remittances from 22 delinquent employers through enforcement actions.
“To further boost or expand our collection, this year, we plan to intensify employer visitation to update records and promote online payment compliance. We will also conduct forums with employers, business permit and licensing offices, and collecting partners to improve remittance compliance,” Almanon shared.
He added that complaint affidavits against delinquent employers will continue to be filed to ensure that employees receive the benefits they are entitled to.
To facilitate seamless contributions, PhilHealth is promoting the use of its Electronic Premium Remittance System which is an online platform that allows employers to submit contributions more efficiently.
“No Central Luzon resident should have to worry about unpaid hospital bills. We are committed to delivering fast and reliable services so that hospitals and patients alike can benefit,” Almanon pressed.
He added that through faster claims processing and strengthened collections, the agency is securing the future of UHC in the region.
Meanwhile, PhilHealth has reinforced its No Co-Payment Policy to protect patients from excessive charges, ensuring that members in public hospital wards do not pay beyond the state-owned firm’s set rates.
The agency is also encouraging all members to stay informed about their claims and benefits.
For inquiries, employers and members may contact PhilHealth’s hotline at 8662-2588 or visit www.philhealth.gov.ph. (CLJD/MJSC, PIA Region 3-Pampanga)